
Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.
Menu
Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.
Pancreatic ductal adenocarcinoma (PDAC) is considered one of the most aggressive and malignant cancer types due to its low survival rate (9% survival within five years) and high metastasis rate. Its complex tumor microenvironment is significantly resistant to several treatment methods, including surgical removal of the tumor. This necessitates a comprehensive understanding of the differentiation in the PDAC tumor microenvironment and the immune-suppressive networks involved.
A closer look into the PDAC microenvironment reveals an abundance of myeloid cells with a variety of characteristics. While dendritic cells (DCs) exhibit antitumor activity by activating cytotoxic T cells that inhibit tumor progression, tumor-associated macrophages (TAMs) promote tumor growth and resistance to immune response.
Although both cell types derive from infiltrating monocytes, the mechanisms by which they differentiate into either TAMs or DCs are not clear.
Glycosylation patterns have been frequently investigated in cancer research. It has been discovered that the sugar chains of surface proteins and lipids are significantly altered in tumor cells. More specifically, glycans on healthy cell surfaces comprise long sugar chains added by glycosyltransferases. On the other hand, the chains of tumor cell glycans are truncated with sialic acid addition catalyzed by sialyltransferases. The hypersialylated glycans are associated with the upregulation of oncogenes, especially in breast, colon, and prostate cancer (1)(2)(3).
The recognition of sialylated glycans by sialic acid–binding immunoglobulin-type lectins (Siglecs) has been linked to the immunosuppressive properties of tumor microenvironments, such as an increase in Treg cells and reduction in T cells (4).
Considering the expression of various Siglecs on PDAC monocyte surfaces, researchers from Vrije Universiteit Amsterdam hypothesized that the sialic acid–Siglec interaction could facilitate monocyte differentiation to an immunosuppressive phenotype (5).
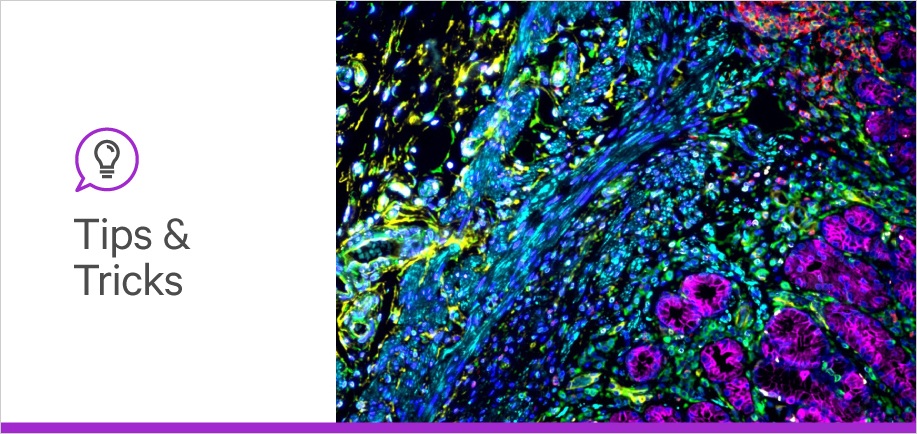
The researchers first confirmed the increased expression of sialylated glycans in PDAC through gene set enrichment, immunohistochemistry with sialic acid–specific plant lectins from Vector Laboratories, and flow cytometry. Then, they determined whether these glycans served as ligands for Siglec receptors.
The myeloid cell characterization was done by analyzing the siRNA-seq data from Peng et al (6). Further gene set enrichment analysis was performed to reveal the main factors behind the low survival rate and the underlying mechanism behind the specific differentiation type. The monocyte differentiation was also monitored in cell co-culture systems with pancreatic tumor cell lines.
To evaluate the association between sialylated glycans and monocyte-to-TAM differentiation, the researchers blocked the glycan–Siglec interaction with Siglec-blocking antibodies. Then, they monitored the cell markers specific to differentiated monocytes. Throughout the lectin staining experiments, Vector Laboratories’ Carbo-Free Blocking Solution was used to eliminate background signals caused by glycoprotein contamination.
Enhanced Sialic Acid Expression
Sialylation is enhanced in pancreatic tumor cells, where sialic acids form glycosidic linkages with glycan chains in the presence of sialyltransferases. In gene set enrichment analysis, the main sialylated glycans were α2,3- and α2,6-linked. In parallel with these results, the gene expressions of enzymes responsible for the synthesis of sialyl-t and sialyl Tn antigen (ST3GAL1 and ST6GALNAC1, respectively) also increased in PDAC cells.
Investigation of PDAC patient biopsies confirmed the increased expression of α2,3- and α2,6-linked sialic acids. To detect α2,3- and α2,6-linked sialic acid residues, Vector Laboratories’ plant lectins Maackia amurensis (MAL II) and Sambucus nigra (SNA), respectively, were used to stain the patient biopsies.
Interestingly, the flow cytometry of the surface glycans revealed that α2,3 sialic acid expression was higher in PDAC than in normal cells, while α2,6 expression did not differ between normal and PDAC cells. This demonstrated that α2,3 sialic acid was the more prevalent and significant sialic acid in PDAC tumor formation.
Sialic Acid and Siglec Interactions
The researchers used flow cytometry to measure the affinity of sialylated glycans to Siglecs and found that the glycans in PDAC cancer cell lines had an affinity for Siglec-7 and Siglec-9. The sialylation of these glycans was carried out by ST3GAL1 and ST3GAL4, respectively. In particular, ST3GAL1 was responsible for the α2,3 sialylation of short O-glycan chains in pancreatic tumors.
To find out which specific tumor cells expressed the Siglec-7/9 receptors, the researchers compared single-cell RNA sequencing data of PDAC biopsies and control pancreatic samples. The Siglec expression was enhanced in myeloid cells, which confirmed that the sialylated glycans interacted specifically with the Siglecs found in myeloid cells.
The Differentiation of PDAC Myeloid Cells
After confirming the interaction of sialylated glycans with PDAC myeloid cells, the researchers quantified and characterized the myeloid cell population. The two dominant myeloid cell types in PDAC were monocyte-derived macrophages and monocyte-derived dendritic cells. More importantly, gene set enrichment and survival analysis showed that a higher ratio of macrophages to dendritic cells led to shorter survival. This clearly demonstrated that the most aggressive and malignant PDAC subtype was the one that comprised a high percentage of macrophages, while dendritic cell–dominant PDAC had higher survival rates.
Sialylation and Macrophage Differentiation
The most crucial step to fully mapping monocyte-to-macrophage differentiation was to determine the role of sialylated glycans in differentiation to macrophages or dendritic cells. The researchers accomplished this by blocking certain points along the sialylation pathway. The blockade of Siglec-7/9 binding reduced the differentiation to tumor-associated macrophages.
In another set of PDAC cell lines, the impact of the sialic acid activating enzymes (the step before sialylation) was evaluated with an enzyme knockout. The sialic acid content in PDAC (with or without the knockout) was detected using MAL II lectin staining from Vector Laboratories. Inhibiting sialic acid synthesis led to an absence of sialylated glycans in the cell lines, although this did not affect their macrophage differentiation. This time, however, the macrophages did not express the tumor-associated cell markers in the absence of sialylated glycans.
Not only were the sialylated glycans able to differentiate monocytes into tumor-associated macrophages, but they could also alter the phenotypes of already differentiated myeloid cells. The expression of antitumor cell markers was reduced, while genes associated with immune evasion were upregulated.
The results of the study shed light on altered glycosylation patterns in PDAC. The hypersialylation of glycoproteins and glycolipids in PDAC was strongly correlated with immunosuppressive myeloid cell formation. In particular, the tumor-associated macrophage differentiation was mediated by an increase in sialylated glycan-Siglec 7/9 interactions.
Comprehensive study of the PDAC pathway could open the doors to more effective immunotherapy strategies involving the sialic acid–Siglec axis. In fact, targeting this axis in breast cancer tumors resulted in tumor size reduction in mouse models (7). Targeting similar sialylation networks in PDAC and other treatment-resistant cancers could improve immune response and subsequent therapy outcomes.
References




Stay in the Loop. Join Our Online Community
Together we breakthroughTM

©Vector Laboratories, Inc. 2024 All Rights Reserved.