
Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.
Menu
Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.

Every bit of progress in the research and development of new treatments for spinal muscular atrophy (SMA) counts as a big win. Spinal muscular atrophy is a serious genetic condition that results in the degeneration of motor neurons. As a result, patients with SMA develop muscle weakness, atrophy, and paralysis, eventually leading to death (1). A cure for SMA is currently unavailable, but different treatment approaches can come together to advance the management of SMA symptoms and improve patients’ quality of life.
SMA is a rare disease caused by a deletion or mutation to the survival motor neuron 1 (SMN1) gene. It affects 1 to 2 individuals per 100,000 newborns (1). Without adequate levels of SMN protein, motor neurons cannot survive, and thus, muscles can’t function (1). Although patients with SMA still have the SMN2 gene, they don’t express enough SMN protein to support motor neuron viability and muscle function (1).
SMA phenotypes are classified into 4 types according to the age of onset, the level of motor dysfunction, and the age at death (1):
Although a cure for SMA is currently unavailable, the Food and Drug Administration (FDA) has approved some interventions, including gene therapy with onasemnogene abeparvovec (2). This therapy uses a virus that crosses the blood-brain barrier to deliver a functional copy of the SMN gene to target motor neurons. Clinical trial data show that intervention improves symptoms, and infants who receive onasemnogene abeparvovec live longer and have a reduced need for respiratory support than non-treated patients (3,4). Some infants could sit unassisted, and a few could even walk (3,4).
Keep reading to learn more about research done with specimens from patients who received abeparvovec and another SMA-related preclinical study. If you want to read about scientific advances in additional fields of research, check out other publication highlights here on the blog.
Despite available evidence confirming clinical efficacy, few studies have investigated the distribution of the vector genome across different tissue types and its impact on the expression of the SMN protein after treatment with onasemnogene abeparvovec. Intending to fill this gap, Thomsen et al. used post-mortem tissue to investigate the biodistribution of the SMN gene and protein across the central nervous system (CNS) and peripheral organs (5). Researchers used post-mortem specimens from patients who had SMA type 1 (SMA1), received onasemnogene abeparvovec (single intravenous administration), and died of treatment-unrelated respiratory complications. One of the two patients experienced an improvement in motor function while the other died shortly after administration and didn’t show any clinical improvement. The research team then used various molecular and cellular techniques to investigate the biodistribution of the vector genome, mRNA transcript, and SMN protein in multiple tissues. Results showed that the vector genome was present in motor neurons from both patients. Other CNS (brain and spinal cord) and peripheral (muscle, liver, and thymus, among others) tissues also contained the vector genome. Next, Thomsen et al. observed that onasemnogene abeparvovec mRNA transcript was present in tissue samples from only one patient, as mRNA degradation likely prevented detection in specimens from the other patient.
Classic immunohistochemistry techniques then allowed the researchers to assess the distribution of SMN protein in various tissues. They analyzed specimens from patients with SMA who didn’t receive treatment and one patient without SMA1. Preparation of samples from different patients included formalin-fixed paraffin embedding or flash-freezing followed by post-fixation. Following subsequent steps applicable to each preservation technique, samples were blocked to reduce non-specific binding and incubated with a specific primary antibody. Researchers then used biotinylated goat anti-mouse secondary antibody, a VECTASTAIN® HRP- ABC Kit, and a Vector® NovaRED™ Substrate Kit to detect the target SMN protein. Results revealed that patients with SMA1 who received treatment expressed more SMN protein in spinal cord motor neurons than non-treated patients with SMA1. Immunostaining also revealed that patients who received onasemnogene abeparvovec also expressed the SMN protein in neuronal and glial cells in other CNS regions.
Thomsen et al. also assessed the expression of the choline acetyltransferase (ChAT) enzyme, a motor neuron-specific marker, in tissue from treated and non-treated patients with SMA. Following steps similar to the ones performed for immunodetection of SMN protein and swapping the choice of biotinylated secondary antibody for horse anti-goat, they observed that ChAT was absent or expressed at low levels in control SMA tissue. However, in tissue from patients with SMA who received treatment, the number of ChAT-positive motor neurons doubled relative to untreated patients. Despite this significant increase, the number of ChAT-positive motor neurons in treated tissue was still half that observed in non-SMA control tissue.
Data from Thomsen et al. represent significant progress in SMA research. Even though results don’t translate as a cure or long-term clinical management for this disease, they show that it’s possible to use a vector genome to increase the expression of the SMN protein, resulting in detectable yet limited improvement of motor function. The development of pharmacological interventions targeting other aspects of the SMA pathophysiology can further improve the management of SMA symptoms. Simon et al. have shown that pharmacological increase of neuronal activity can help improve motor neuron function in a preclinical model of SMA (6).
During development, neuronal activity is essential for the formation, refinement, and maintenance of the connection between motor neurons and muscle fibers. Various molecular signals attract the motor neuron to the muscle fiber, and neuronal activity strengthens and maintains the neuromuscular junction (NMJ). However, the contribution of neuronal activity (or lack of it) to the progression of SMA is an unexplored topic. Simon et al. explored the impact of pharmacological manipulation of neuronal activity on synaptic function at the NMJ in an animal model of SMA (6). They used 4-amino-pyridine (4-AP), a drug that promotes the efflux of potassium, to increase neuronal activity and hypothesized this intervention could ameliorate some of the muscular dysfunction (6).
Mice don’t have the SMN2 gene, thus, generating a preclinical model for SMA required deleting the SMN1 and adding the SMN2 gene that expresses full-length SMN at low levels (7). Motor neurons in the resulting SMAD7 mouse model exhibit low activity levels, which leads to muscle dysfunction and eventually neuronal death (8–10). In Simon et al.’s study, a single intraperitoneal injection of 4-AP in SMA mice increased the expression of c-Fos, a marker for neuronal activity, in motor neurons, other spinal cord neurons, and dorsal root ganglia sensory neurons (11). Next, chronic intraperitoneal administration of 4-AP (twice a day; from birth to death) improved motor reflexes, ability to walk, and survival in SMA mice. Wild-type mice, however, didn’t show changes in motor reflexes, body weight, and survival after receiving chronic 4-AP. It’s important to note that the improvement observed in SMA mice was independent of SMN protein expression, as its levels didn’t change in response to treatment. Chronic 4-AP administration didn’t prevent or delay neuronal loss either.
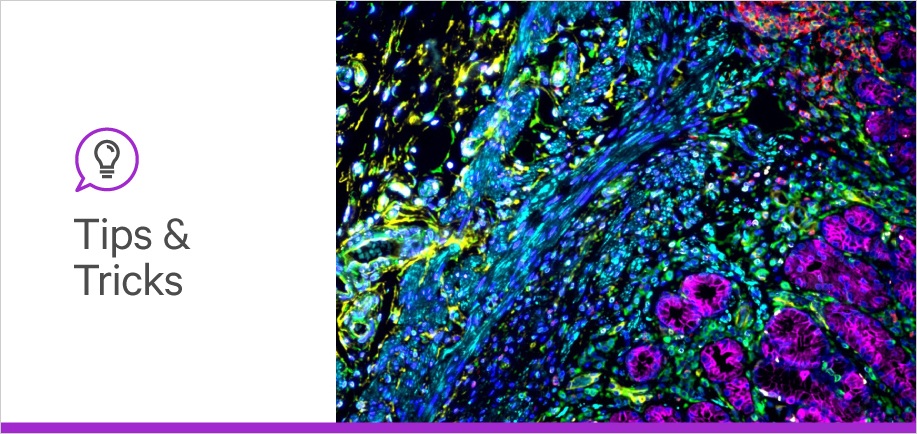
The next logical question became: What are the changes underlying the functional improvement observed after chronic 4-AP administration? To answer this question, researchers used confocal microscopy to assess changes in the number of synapses between motor neurons and muscle fibers. They used VECTASHIELD® PLUS Antifade Mounting Medium to help prevent photobleaching while acquiring z-stacks. Quantitative analyses of photomicrographs revealed that boosting neuronal activity with 4-AP promotes axonal sprouting, or in other words, increases the number of synapses at the NMJ. However, significant increases only happened at later stages of development (P11), not earlier stages (P6). These data indicate that neuronal activity-induced axonal sprouting can compensate for the loss of motor neurons in SMA, resulting in motor function improvement.
Simon et al. had previously shown that inhibition of the p53 pathway with PFT (Pifithrin-a) prevents death of motor neurons but has no effect on the number and function of synapses (12). Could co-treatment with 4-AP and PFT have an additive effect? In a final experiment, researchers performed daily co-injection of 4-AP and PFT in SMA mice (from birth through death) and observed full correction of the synaptic response. These results suggest that multiple interventions can come together to counteract different aspects of SMA pathophysiology.
Gene therapies are promising interventions to treat SMA, and the Thomsen et al. study showed that this approach can change the patients’ phenotype and increase expression of SMN in motor neurons. Most importantly, the treatment increased neuronal viability and helped patients reach important motor milestones. As research and clinical management of SMA continues to evolve, the development of adjunctive therapies may significantly improve patients’ quality of life. Data from Simon et al. exemplifies how targeting neuronal activity at the NMJ and the p53 pathway can improve functional outcomes. Tackling different aspects of the SMA pathophysiology can help the scientific and medical communities reach the long-term pursuit of finding a cure for SMA.
Vector Laboratories is proud to empower scientists to move knowledge forward. Check out our learning resources and reach out to our team of experts if you need technical assistance with your experiment and reagent selection.




Stay in the Loop. Join Our Online Community
Together we breakthroughTM

©Vector Laboratories, Inc. 2024 All Rights Reserved.