Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.
Menu
Vector Laboratories is closed for the President’s Day on Monday, February 19th. We will be back in the office on Tuesday, February 20th.
We will respond to emails upon our return. Have a wonderful day.

Alzheimer’s disease (AD) is a progressive neurodegenerative condition that leads to brain atrophy, memory loss, and confusion. Scientists continue to search for the answer to many unresolved questions in the pathophysiology of AD. One of those areas revolves around the factors contributing to selective neurodegeneration—the observation that some cells die while others remain resilient (1). This selective vulnerability is characteristic of many neurodegenerative diseases and, in AD, has been observed in some neuronal populations in the hippocampus (2–4). The factors underlying selective neurodegeneration are mostly unknown, and discoveries in this area may directly impact the development of new therapies for AD.
Using single-nucleus RNA sequencing (snRNA-seq), Zalocusky and colleagues showed that expression of apolipoprotein (Apo) E in neurons could be one of the factors contributing to selective vulnerability in AD (4). Data from their study provide robust evidence that increased levels of ApoE in neurons drive the expression of immune function genes, contributing to morphological and functional changes characteristic of AD.
Keep reading to understand the details of this valuable scientific discovery as we highlight impactful research for Alzheimer’s Awareness Month.
In the search for common characteristics of the vulnerable neuronal population, Zalocusky et al. focused on the pathological role of ApoE. As with any other lipoprotein, ApoE plays a vital role in lipid metabolism. In the brain, ApoE is mainly produced in astrocytes. Its neuronal expression associates with stress, injury, and aging and contributes to impaired synaptic plasticity, tau pathology, learning, and memory deficit. Different isoforms—ApoE2, ApoE3, and ApoE4—have been characterized, of which ApoE3 is the most common (9). Humans carrying the allele for ApoE4 have an increased risk for AD and decreased age on onset (2,3,10). Expression of human ApoE4 in mouse models results in tau pathology, neuroinflammation, and neuronal loss (11).
To identify common factors that could potentially associate with selective vulnerability, Zalocusky et al. performed gene profiling in various neuronal populations. They dissected hippocampi from female mice expressing human ApoE3 (ApoE3-KI) and ApoE4 (ApoE4-KI) and isolated nuclei from various neuronal populations. Using snRNA-seq, Zalocusky et al. analyzed a total of 123,489 nuclei and 21,204 genes. Results revealed a total of 27 clusters of cells, with 16 being neuronal clusters. Regression analyses showed that ApoE expression explained 59–82% of within-cell variability depending on the cell cluster. Researchers also used to identify other functional pathways associated with ApoE expression. Results revealed that ApoE correlated with genes involved with metabolism, neurodegeneration, cellular senescence and apoptosis, DNA damage and repair, immune response, autoimmunity, and response to infections.
Using animal models to investigate the mechanisms underlying disease pathophysiology is a convenient approach that gives the investigator total control over the experimental design. However, when the long-term goal of a research study is to inform the development of new therapies, examining whether the data replicate in humans is essential. Zalocusky et al. profiled gene expression in neuronal cells from the brains of patients with mild cognitive impairment or Alzheimer’s dementia. Results showed that, on average, 28% of neurons expressed ApoEvaried with age and disease stage. Similar to animal model findings, pathway analysis in human cells revealed that ApoE expression correlated with genes associated with cellular metabolism, neurodegeneration, DNA damage and repair, immune response, autoimmunity, and response to infections. Together, gene profiling data suggest that neuronal ApoE expression is potentially an important driver of within-cell-type variability in both mouse and human brains.
Next, Zalocusky et al. assessed ApoE expression in neurons from ApoE3-KI and ApoE4-KI mice at different ages. They observed that the proportion of neurons expressing high levels of ApoE peaks at a specific time and then goes down. In ApoE3-KI mice, the peak happened at 20–21 months, and in ApoE4-KI mice, at 15–16 months. The authors suggest that the decline in the proportion of neurons expressing high levels of ApoE after its peak could indicate that ApoE expression drives neuronal loss.
Researchers also showed that this temporal change in ApoE expression follows a similar pattern in neurons from human brain cells. They observed a low proportion of neurons expressing high levels of ApoE in individuals with no cognitive impairment. Patients with mild cognitive impairment had the highest proportion of neurons expressing high levels of ApoE. Mild cognitive impairment often develops in the early stages of AD and is characterized by memory or thinking problems such as forgetting events or appointments, trouble navigating familiar locations, and a hard time finding the right word to express an idea or thought (12). As AD progresses, cognitive impairment becomes more severe and patients develop dementia. In patients with AD, Zalocusky et al. observed a relatively low proportion of neurons expressing high levels of ApoE. Data from human brain cells support the same conclusions drawn from animal data. Neuronal ApoE expression increases during the early stages of AD and declines as the disease progresses. Could ApoE be one of the driving factors of neuronal loss in AD?
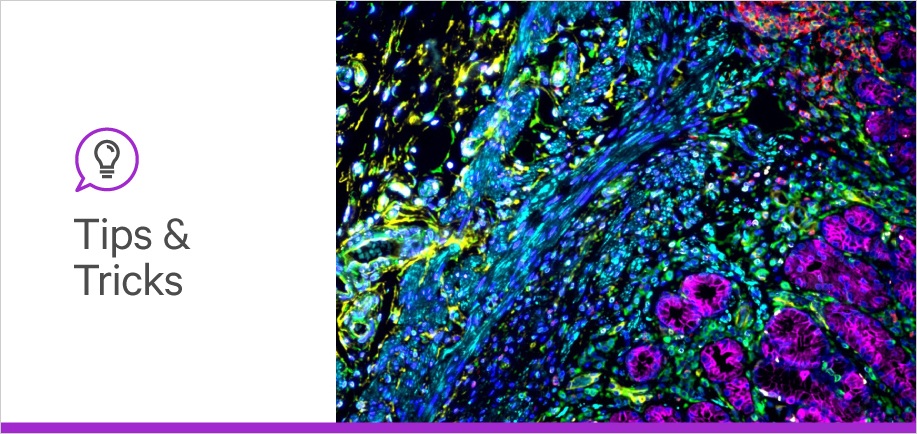
Following the above study, Zalocusky et al. turned off the expression of human ApoE in neurons and investigated its impact on neuronal and synaptic loss. All the other cell types in the conditional knockout mouse model continued to express human ApoE. Age-matched mice expressing human ApoE served as controls for this experiment. Then, they used immunohistochemistry for NeuN (a neuron-specific marker) and PSD95 (a protein essential for the formation of synapses) to quantify changes in neuronal and synaptic density, respectively As some of the antibodies used in the immunohistochemistry were raised in mice, researchers used M.O.M.® (Mouse-on-Mouse) Blocking Reagent to optimize the staining and reduce unspecific background. After incubating the slices with appropriate secondary antibodies and mounting the slides with VECTASHIELD® Antifade Mounting Media with DAPI, Zalocusky et al. quantified NeuN+ cells and PSD95 immunofluorescence intensity. Data showed that neuron-specific knockout of the ApoE gene results in higher neuron density, larger hippocampal volume, and preservation of synaptic proteins.
Initial pathway analysis revealed that ApoE expression in neurons strongly correlated with immune function-related genes. Within those, MHC genes showed a prominent correlation with ApoE expression on a cell-by-cell basis. Lack of ApoE expression resulted in the downregulation of MHC gene expression at both RNA and protein levels. Functional expression of MHC-I genes requires the protein B2M (15,16). As a next step, Zalocusky et al. silenced B2M expression in primary neurons expressing human ApoE4, which are cells that accumulate phosphorylated tau in the neuronal soma (15,17). Knockdown of B2M resulted in reduced expression of B2M and MHC-I, but most interestingly, also reduced phosphorylated tau in the soma primary neurons expressing human ApoE4. As expected, ApoE4 expression remained unaltered.
Zalocusky et al. also induced the expression of human pathological tau in wild-type and B2M-knockout mice. Researchers used immunostaining followed by impregnation to detect tau pathology in brain slices. The use of Avidin/Biotin Blocking Kit and a ensured low background and optimal staining, and results showed that B2M-knockout mice had reduced tau pathology. Lastly, Zalocusky et al. observed correlations between MHC-I genes and tau tangle pathology in humans. Regression analysis revealed that MHC-I expression predicts tau pathology in human brains even when controlling for age, sex, ApoE genotype, ApoE level, and AD clinical status.
The Zalocusky et al. study provides robust evidence that ApoE expression in neurons drives activation of the immune response and selective vulnerability in AD. The cascade of events that unfolds after neuronal expression of ApoE includes expression of MHC-I, tau pathology, synaptic dysfunction, and neuronal loss. Overall conclusions come from data gathered from human samples and animal models, strengthening the findings’ translatability. As with any discovery, many questions remain unanswered. For example, what triggers ApoE expression in neurons? Are there other components mediating the relationship between ApoE and neuronal loss? Despite unanswered questions, these data provide new mechanistic insight into the pathophysiology of AD, which opens the possibility for new treatments. New therapies could individually target different components of the newly discovered cascade. However, the authors suggest that the best results would likely come from an intervention that combines multiple drugs targeting different components of the ApoE-MHC-neuronal loss axis.
If you want to learn about other innovative findings, check out other publication highlights, and be sure to stay tuned into the blog for more insights.


Stay in the Loop. Join Our Online Community
Together we breakthroughTM

©Vector Laboratories, Inc. 2024 All Rights Reserved.